Pre-conception and fertility with chronic illness - what my 2 year journey looked like
The timeline no one talks about when you have a chronic illness
Thank you for reading. Please hit the heart button to show your support ♥️
Hey Homebodies,
Lucy here 👋
I’m going to start this out by highlighting a trigger warning for fertility, pregnancy and chronic illness.
Sharing my experience with fertility and chronic illness has honestly been super taxing for me to write and relive, but I think it’s incredibly important to share, especially for those who are going through a similar situation.
When I was going through my experience, it felt isolating, lonely and overwhelming, and I wish I could have found content that could make me feel seen, like this piece I’m about to share with you.
If you aren’t interested in this topic, but know someone who is or may go the intersection of chronic illness, pre-conception and fertility it in the future, please forward or link them to this piece. I am always open to answering any questions and will continue to update this resource.
And a quick disclaimer: I'm sharing my personal journey here, not medical advice. I'm not a healthcare professional - just someone who's been through this experience. As you'll read below, building the right healthcare team was crucial for me, and I'd encourage you to do the same for your unique situation. Take what feels relevant to you, leave the rest, and always work with qualified professionals who understand your specific needs.
Let’s dive in.
This free article is supported by my brand partners:
♥️ Receive 30 days for free with my favourite breathwork & meditation online app, Open
🥬 Receive up to $200 AUD off your first 5 boxes with my favourite pre-made meals by YouFoodz
What We're Covering Today
🚨This is a long article, so if it cuts off you will need to read it in your browser or via the Substack app.
1. Why my fertility timeline extended to 2 years
There's a space between 'thinking about having a baby' and 'trying to have a baby' that no one really talks about. For most people, it might last a few months, for me, it lasted nearly two years.
It all began in 2020 when my body decided to remind me, in the most dramatic way possible, that I don't get to make assumptions about anything, especially not my health or pregnancy.
My partner and I had always talked about children. We were in our late twenties, planning our wedding, full of that naive confidence that comes with youth and good intentions. We'd made all the typical assumptions: get married, get pregnant, it would be super easy. Why wouldn't it be?
Then 2020 happened. COVID, lockdowns, moving from Melbourne to Adelaide, planning a wedding - and my body said absolutely not to all of it.
I started flaring up again. I go through periodic times in my life of flare-ups with my lupus and rheumatoid arthritis, usually connected to stress and lifestyle factors. But this one was different. I honestly thought it would be like the others - rest, painkillers, supplements, and it would pass.
But it didn't pass. It got progressively worse until I was in excruciating, acute pain. The only way I can describe it is like the day I broke my toe (it’s the only bone I’ve broken!), that same bone-breaking level of pain, but throughout my entire body, for months on end. People might think that sounds dramatic, but it's genuinely traumatising. There's something about being in debilitating pain for extended periods that breaks you down in ways you don't expect.
I tried to manage it myself at first. I started seeing a chiropractor, thinking it would help regulate my nervous system like previous gentle practitioners had. But this person was way too intense, too physical, and every appointment left me worse than before. After each session, I'd get flu-like symptoms. I couldn't get out of bed, I had muscle aches, headaches, migraines, joint swelling and sore throats. My immune system was just getting more and more triggered.
When I finally got in to see my rheumatologist after three months on the waiting list, the tests revealed what I'd been afraid to acknowledge - my body was in a bad way. My inflammatory markers were sky high, there was damage to my heart from lupus and my lungs were affected too, though thankfully still strong.
2. When My Doctor Said 'You Can't Get Pregnant Right Now'
Then my rheumatologist said something that changed everything about my pregnancy timeline: "You essentially won't be able to get pregnant. Your body is in way too much stress, too inflamed, struggling too much just to survive. There's just no way you can or should get pregnant anytime in the near future".
He wasn't being cruel. He was being honest. My body was so focused on basic survival that reproduction wasn't even on the table. And if I somehow did get pregnant in that state, it would be dangerous for me and for the baby.
Initially, he wanted me on methotrexate, an oral chemotherapy drug. I had been on it in a trial when I was 7 years old. Back then it left me nauseous and weak.
I agreed at first, I felt so hopeless and overwhelmed with pain that I was agreeing to anything at that point, but as I got home, something in my gut said no. I called him back to discuss it further, and that's when I learned the full implications: not only could I not get pregnant while on it, but different doctors had different opinions about how long to wait after stopping, anywhere from three months to a year.
To be honest in my mind, I was still in denial over how bad the state of my body was, even though I was being told my organs were being damaged, I had this strange hope that I would wake up the next day and my flare-up would be over. So, the thought of pushing out our family timeline by years felt impossible to accept. I begged/negotiated: could I try a combination of prednisolone (a steroid) and Plaquenil instead? (I had been on this combo in my early twenties with success).
He agreed, but would only give me three months, which would be the time it would take for Plaquenil to build up in my system. If I wasn’t seeing positive signs towards the flare-up being under control, I would need to resort back to methotrexate to not further damage my organs and body.
3. 8 months of intensive health management before trying
What followed was eight months of intensive health management that had nothing to do with fertility and everything to do with basic survival and damage control.
I assembled a team: my rheumatologist, a nutritionist specialising in autoimmune conditions, a physio, and eventually a GP who specialised in women's health. We did comprehensive testing that Western medicine often skips, including MTHFR genetic testing. Turns out I have one of the most significant types, a double mutation that means my body can't process regular folate, which would be crucial for pregnancy.
I was also dealing with low iron, low vitamin D, and low magnesium. I started a supplement regime that included fish oil, iron, vitamin D, magnesium, resveratrol, probiotics, NAC, SPM Active (and others I'm probably forgetting).
Beyond supplements, I changed everything. We bought water filters and a Dyson air filter. I went on a strict anti-inflammatory diet (basically protein and vegetables), cutting out anything processed, reducing dairy, limited alcohol, limited sugar. One coffee was allowed.
My partner and I started doing hot and cold pools every Friday (unless I had my period) which involved specific sequences to reduce inflammation. I was in bed by 10 PM every night, doing yoga, pilates, and walking when I had energy. When I felt stronger, I added some conditioning and strength training, though I'll be honest, I was taking painkillers before and after just to get through it (I don't recommend that to anyone, but I'm telling you how it really was.)
This wasn't about fertility yet. This was about getting my body to a place where pregnancy was even theoretically possible.
4. Moving from survival mode to hope
After eight months, I was finally able to come off the prednisolone and stay just on Plaquenil, which is pregnancy-safe. I also got the ‘ok’ from my rheumatologist to start thinking about fertility. So, that's when my fertility journey actually began.
I started seeing a fertility acupuncturist, herbalist and naturopath who put me on a prenatal designed for my MTHFR mutation. But even then, she said my nervous system was still too activated, too stressed. So for the first four months, we weren't even working on fertility, we were just trying to get my nervous system calm and stable.
She'd place needles behind my ears, on my collarbones, ankles, wrists, my third eye, all focused on nervous system regulation and stress reduction. When I was finally ready to start focusing on fertility specifically, I added more supplements to my regime - Ovarianne to support ovulation, two different types of specialised herbalist drops for hormone support, L-5MTHF and Tresos Pre Natal.
I also added castor oil packs on my womb during certain parts of my cycle, red light therapy at my acupuncturists clinic, always wore socks (TCM believes to keep your womb warm and happy, to wear socks) and continued with my yoga teacher training that I'd started during recovery.
I switched all our cleaning products (I use Koala Eco), makeup, stopped wearing perfume (I loved rose body oil instead) - basically reducing chemical exposure wherever possible. Did you know that IVF clinics actually ban patients from wearing perfume or scented products during procedures because chemical exposure can impact egg and sperm quality? As soon as I found that out, everything had to go.
I changed my diet to include more warming foods, as suggested in Traditional Chinese Medicine. I highly recommend the book ‘Awakening Fertility: The Essential Art of Preparing for Pregnancy’ (by the same author of ‘The First Forty Days’ - a great postpartum book).
I also went deeper into the spiritual and emotional preparation that often isn’t talked about. I started meditating, visualising my baby with a specific technique I found in the book, Spirit Babies.
I did a traditional Casting the Bones Ceremony, in which the facilitator talked about how my Grandma who had passed was talking to her about holding the hands of my two future children. She said they were safe, but very eager to meet me. The facilitator also talked about how I had to focus on my mother’s lineage and how this would unlock the things I needed to understand to move forward in life.
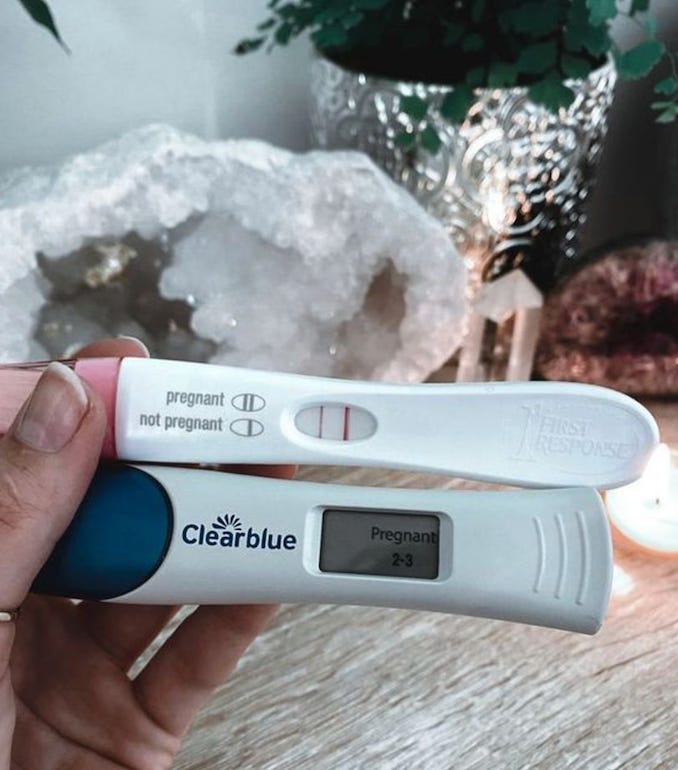
And something that might sound a bit intense: my TikTok algorithm became full of people with positive ovulation and pregnancy tests because that's what I was engaging with. I created a vision board in Canva (one in a landscape spec for my laptop and one for a phone screen spec). I screen-shotted a positive pregnancy test and added it to my vision board (the actual one is below!) Looking at it every day and intensely visualising how I would one day look down at my test, and see the positive sign.
5. The moment we shifted from hoping to actively trying
The conversation with my partner about moving from "if it happens, it would be great" to "let's actively try" was actually pretty relaxed. It was definitely led by me, because I'd spent years working toward the goal of not being in a flare-up and being able to get pregnant. When I felt ready, mentally and physically, I just said, "Okay, I think I feel ready now to try, not just hope it'll happen."
In my journey I was told by many practitioners that I should be prepared to not be able to conceive naturally. That it would be hard with how much damage my body has undergone, and that I should be ready to have help with IVF.
It sounds super unemotional (and honestly I was probably detached and a bit dissociated at the time), but the main difference in my readiness wasn't some magical feeling of completeness. It was practical: I knew that to access IVF, we'd need 12 months of documented trying. And honestly, I was convinced we wouldn't be able to conceive naturally, so I wanted that official start date.
My husband handled the entire extended timeline with incredible grace and patience. His priority was supporting me and looking after me, and I really appreciated that throughout what became a two-year journey from flare-up to positive test.
6. 6 Months of tracking, testing, and the two-week wait
For anyone who's been through intentional conception attempts, you know how consuming it becomes. Spoiler alert: our ‘official’ trying was for dix months, and I honestly don’t know how much longer my mental health would have been able to last.
Those six months of rigorous trying, with ovulation tests (why do we not talk about how much they suck?), specific tracking, timing everything perfectly, it can take over every piece of your mind, body, and soul.
The worst part is that two-week wait between ovulation and when your period is due. It's the most insane in-between time, hoping you'll get a positive test. I was testing way earlier than recommended, starting about five days after ovulation, getting negative after negative.
And in the background was always the knowledge that we'd been told it might not happen naturally because of my lupus, that we'd most likely need IVF.
7. What 'readiness' actually means with chronic illness
Living in the pre-conception space for two years taught me that readiness isn't a feeling, it's a foundation. It's not about achieving perfect health or eliminating all uncertainty. It's about creating the most supportive conditions possible for your unique situation.
For those of us with chronic illness, that foundation-building takes longer, costs more, requires more coordination, and asks more of our partners.
The questions that mattered weren't "are you ready?" but …
Is your body as stable as it can be?
Do you have the support systems in place?
Are you prepared for this to look different than you originally imagined?
While my story involves specific medical complexities, the emotional landscape of extended pre-conception is more common than we talk about. Whether it's chronic illness, financial considerations, relationship timing, career transitions, or just the honest acknowledgment that you need more time to prepare, many of us live in that in-between space longer than we expected.
Your timeline doesn't need to match anyone else's expectations. Your readiness doesn't need to look like the readiness you imagined when you were making assumptions about how easy it would all be.
If you're in this space right now, know that your timeline, however long it needs to be, is valid.
What resonated most with you in this piece? Are you living in your own pre-conception space right now? I'd love to hear from you in the comments or by hitting reply… this conversation matters, and your experience matters too.







This is powerful! Currently in the midst of my chronic health “vs” fertility struggle as well, and it is beyond validating to hear & feel like I’m not the only one - or going through this alone!
Another great read. Thank you for the courage to share this with us, it's always incredibly interesting